Living with Food Allergies

Eosinophilic Esophagitis (EoE)
Eosinophilic esophagitis [EE-oh-sin-oh-FILL-ick uh-sof-uh-JIE-tis] is a chronic (long-term) allergic or immune condition that causes swelling in your esophagus. It is called “EoE” for short. EoE affects people of all ages, genders, and ethnic backgrounds. About 1 in 2,000 people have EoE.1
What Is Eosinophilic Esophagitis (EoE)?
EoE causes swelling in your esophagus. The esophagus is in an upper part of the gastrointestinal (GI) tract (gut) and is the tube that moves food from your mouth to your stomach when you swallow. EoE happens when a large number of white blood cells called eosinophils [EE-oh-sin-oh-FILLS] collect and cause damage in the lining of the esophagus.
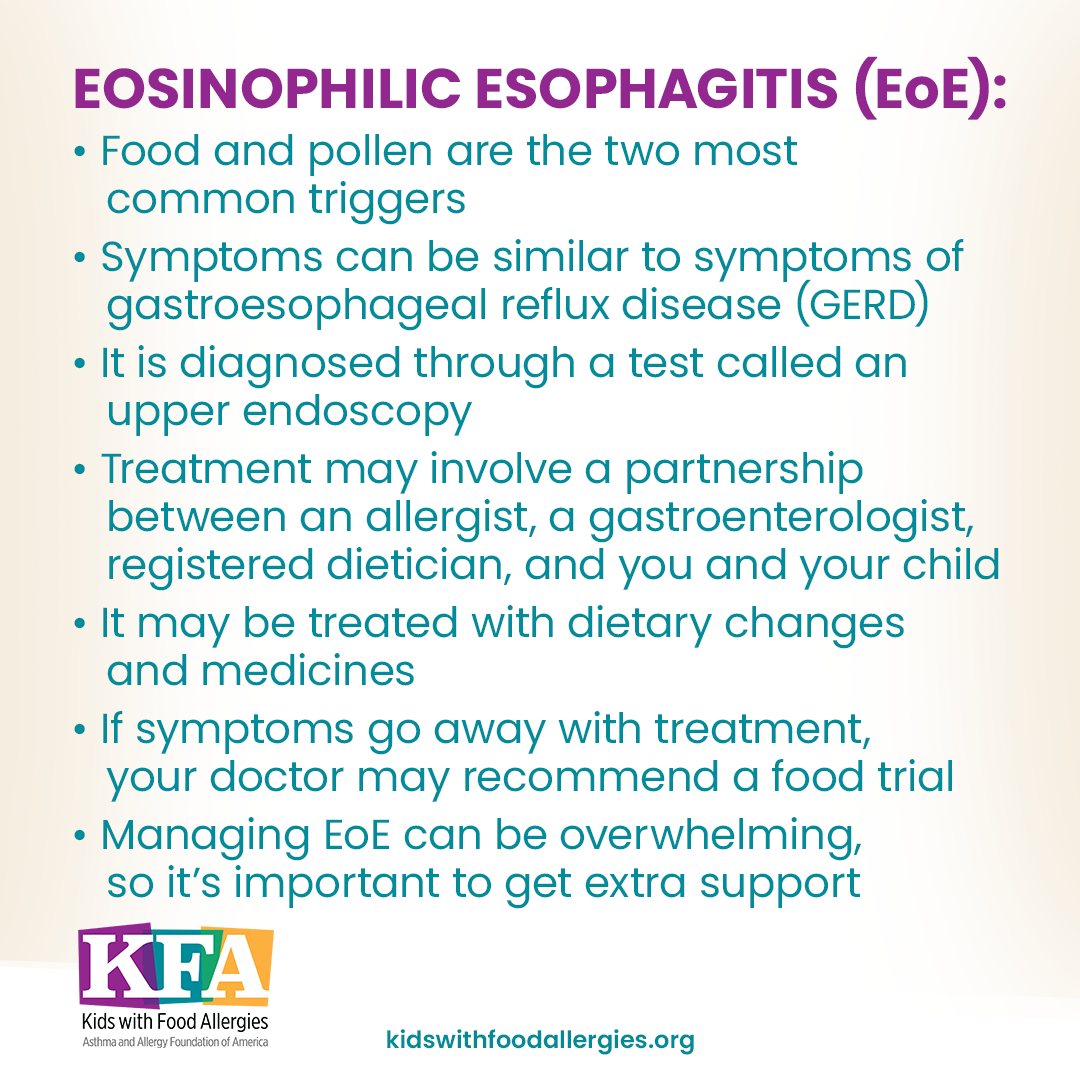
EoE may potentially result from an immune response to food. In some cases, environmental allergens (such as pollen, mold, dust mites, etc.) can also trigger EoE. Sometimes, triggers are not clearly identified.
White blood cells are an important part of our immune system. Eosinophils are a special type of white blood cell. They help us fight off certain types of infections, such as parasites, hookworms, or bacteria. Eosinophils also are involved in other conditions, such as allergies, asthma, and cancer.
Eosinophils serve many roles. Some roles are specific and some are not. This means there are many different processes in the body that can cause eosinophils to be present and/or elevated. Eosinophilic disease may be present when you or your child has high eosinophil counts in the blood or part of the body for a long period of time without a known cause.
Eosinophils can be present in different areas of the GI tract. But eosinophils in the esophagus are not common. Doctors look at the number of these cells in the lining of the esophagus to diagnose EoE.
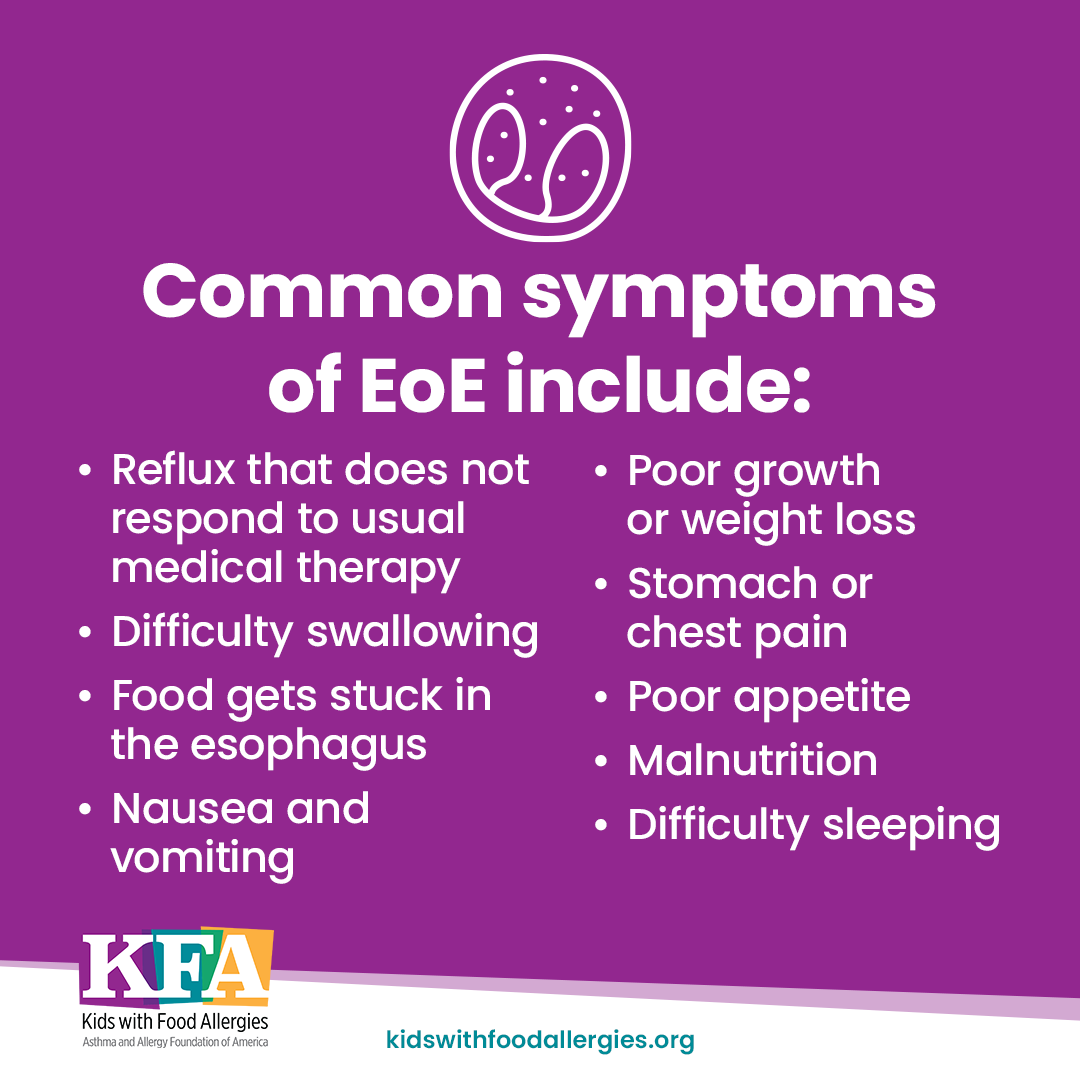
What Are the Signs and Symptoms of EoE?
Symptoms vary from one person to the next, and they may be different depending on age. Symptoms can occur days or even weeks after eating a food allergen. But symptoms may also come and go.
Common EoE signs and symptoms in infants include:
- Poor appetite and won’t feed
- Coughing with feeding
- Reflux that isn’t helped by medicine
- Nausea and vomiting
- Spitting up while arching the back (a sign of pain)
- Poor growth, weight loss, malnutrition
Common EoE signs and symptoms in children include:
- Trouble swallowing or a feeling of food getting stuck
- Food flows back into the esophagus (regurgitation) with reflux that medicine often doesn’t help
- Nausea and vomiting
- Getting full early while eating
- Older children may have chest pain and impaction (food gets stuck in the esophagus)
- Failure to thrive (poor growth or weight loss)
- Stomach pain
Common EoE signs and symptoms in adults include:
- Trouble swallowing
- Food gets stuck in the esophagus (impaction)
- Food flows back into the esophagus (regurgitation) with reflux that medicine often doesn’t help
- Chest pain
- Heartburn
Who Is At Risk of Developing EoE?
EoE can affect anyone. Males are at a higher risk. In some families, EoE may be passed down through genetics.
EoE has a strong connection to allergies. It is common for people with EoE to have other allergic diseases usually caused by type 2 inflammation. These include asthma, allergic rhinitis, or eczema. When you have type 2 inflammation, you may have more than one allergic condition. Not all people with EoE have underlying allergies. In some families, several family members may have EoE.
How Is EoE Diagnosed?
EoE cannot be diagnosed by symptoms alone. While your primary care doctor can refer you to a specialist (allergy or gastroenterology) to assess your symptoms, the formal diagnosis of EoE is done by a gastroenterologist (GI doctor) using a test called an upper GI endoscopy, or EGD. You might hear it referred to as a “scope.” During this procedure, the doctor will take photos and small tissue samples, or biopsies, of the esophagus (and possibly stomach and small intestine) to look for eosinophils.
A pathologist reviews the tissue samples under a microscope. If the biopsies show 15 or more eosinophils, then this would meet the criteria for an EoE diagnosis.
When the doctor performs these tests, the surface of the esophagus may appear very red and swollen. It could be very narrowed (esophageal rings and or strictures). It could have many white bumpy patches. It might even have an accordion-like appearance.
EoE can be tricky to diagnose for many reasons:
- Symptoms can vary from person to person and between age groups.
- People with EoE may have learned to manage their symptoms. They may cut food into smaller pieces, drink liquids when eating dry foods, put off meals, and avoid pills.
- Eosinophils can be found in the esophagus for other diseases, such as:
- Gastroesophageal reflux disease (GERD)
- Other forms of esophagitis that damage the lining of the esophagus
- Infection
- Inflammatory bowel disease
If EoE goes untreated, it can lead to long-term damage to the esophagus. The tube can narrow and tighten – called a stricture – which can make it harder to swallow and pass food through to the stomach. The esophagus may need to be stretched by a GI during an endoscopy.
GERD typically causes far fewer eosinophils in the esophagus than EoE. Currently, experts have not determined what range of eosinophils indicates severe reflux or a process that may respond best to anti-acid medicine, and what range clearly indicates EoE. Unfortunately, no other cell or tissue findings have been identified to help clarify this situation.
How Is EoE Treated?
There is no cure for EoE, but you can manage it. A team of health care professionals can work with you to help you manage EoE:
- Allergist and immunologist
- Gastroenterologist
- Primary care doctor (including pediatrician or family medicine)
- Nurse
- Dietitian
- Psychologist, therapist, or counselor
Your health care team can help you set your goals for treatment. They will likely include:
- Helping heal the lining of the esophagus
- Managing existing narrowings (“strictures”) of the esophagus
- Preventing or reducing risk of long-term complications
- Improving symptoms and quality of life
EoE is treated through a combination of diet changes and medicine to control the inflammation.
Dietary Changes for Treating EoE
EoE may sometimes be triggered by food. Many children and adults with EoE respond well to changes in their diet. Dry or dense foods may be hard to swallow until the esophagus is healed.
There are different versions of elimination diets which may involve removing one, two, four, or as many as six food groups from your diet. Your doctor can help you decide if you need an elimination diet.
There are three main types of dietary therapy for EoE:
1. Empiric elimination diet – This is a treatment that involves avoiding major food allergens. Your doctor may have you try this diet without allergy testing. There are different versions of this diet. The six-food elimination diet removes milk, egg, wheat, soy, nuts, and seafood. Another version removes four allergens: milk, egg, wheat, and soy. Or your doctor might have you remove only cow’s milk. According to studies, the four-food elimination diet is the most effective dietary therapy for EoE.2
Certain people with EoE improve after removing animal milk from their diet. If symptoms persist after removing milk, you may need to avoid additional foods, such as wheat, eggs, soy, peanuts/tree nuts, and fish/shellfish. However, there is no evidence that starting with just milk elimination has better results than starting with a four- or six-food elimination diet.
2. Testing-directed elimination diet – In some cases, food allergy testing may help determine which foods to avoid. Before starting this diet, your doctor will do allergy testing to identify food allergies. Two main types of allergy tests may be used: skin prick tests (“scratch tests”) and specific IgE (sIgE) blood test. Both tests check for specific allergic responses to foods. If you or your child tests positive to a food, the doctor will usually recommend removing that food from the diet. The doctor may also recommend you remove cow’s milk because it can often show as a false negative on allergy tests. More recent guidelines have de-emphasized the role of testing.
3. Elemental formula diet – An elemental diet is a liquid, formula-based diet. In certain cases, more extensive food elimination is recommended. In these cases, the diet is managed with a special non-allergenic formula (a type of medical food). This is most often used in very young infants or in children and adults with more severe disease or malnutrition.The formula is made of special amino acids (protein building blocks) that help avoid allergic responses. They provide complete nutrition while helping you manage EoE. They may be given through a feeding tube. Examples include Neocate®, EleCare®, PurAmino™, Alfamino™.
After some time on dietary therapy, you may be able to add food back to your diet by doing a food trial. In a food trial, you will add food back one ingredient at a time. This helps determine which foods are causing a reaction. Food trials begin after symptoms go away from diet therapy. If symptoms return, the doctor may perform another biopsy to see if eosinophils have returned. It is important to remember that the foods that trigger EoE can change over time.
While diet therapy is often a recommended treatment, it is not the only treatment to consider. Elimination diets may have slightly weaker evidence for effect than use of steroids alone. Diet therapy needs to be very carefully considered in the context of your life and your preferences for how you wish to live your life.
Medicines and Treatments for EoE
While diet changes can help, this is not the only treatment option, and is not always the initial treatment option chosen. Medicines can also help manage and reduce symptoms associated with EoE. Some treatments also target the underlying inflammation that causes EoE. Here are the most common treatments for EoE:
Proton pump inhibitors (PPI)
Older guidelines for EoE treatment recommended doing trial of PPI (for up to 8 weeks) before a diagnosis could be made. These recommendations have changed in recent years and this is no longer necessary. PPIs:
- Are pill or liquid medicines that reduce acid production in the stomach
- Treat acid reflux
- Can reduce eosinophils in the esophagus ( can be used in children as young as 1 year old)
- Can control trouble swallowing
- Are often tried first before elimination diets or steroid treatments because this treatment is available over-the-counter
- Are generally safe, but long-term use may increase risk of nutritional deficiency, gut infections, or bone fractures
Topical corticosteroids
Corticosteroids help control inflammation in the esophagus. The dose sometimes can be lowered to a smaller amount once EoE is under control.
- Corticosteroids are the most used drug treatment for EoE
- Often taken from an asthma inhaler (fluticasone or budesonide) using a “puff and swallow” technique
- Another option is to make a thickened slurry from the liquid medicine that is normally used in nebulizers and then swallow it to coat the esophagus
- Considered safe and are taken at doses similar to asthma – like any steroid, this should be monitored by a doctor because of concerns for an higher risk of thinning bones, mood problems, infections, or diabetes
Esophageal dilation
Over time, EoE can cause scarring in the lining and narrowing of the esophagus, making swallowing difficult. Dilation:
- Helps enlarge the space in the esophagus in people with EoE-related strictures or recurring problems with swallowing to make swallowing easier
- Is a procedure that is usually well-tolerated
- Improves symptoms in nearly nine of 10 people but doesn’t improve the number of eosinophils that cause inflammation
Biologic therapy
Biologics are a type of treatment that target a specific cell or protein to block inflammation pathways.
- Dupilumab (DUPIXENT®) is approved by the Food and Drug Administration (FDA) for people 12 and older with EoE weighing more than 88 pounds
- Indicated as a possible first- or second-line therapy
- DUPIXENT® comes in a pre-filled syringe or auto-injector and given by a doctor in the office or self-administered at home
- Dupilumab side effects include injection site reactions, respiratory infections, joint pain, conjunctivitis (eye infection or inflammation), and herpes viral infections
Nutrition with EoE
Nutrition is critical for people with EoE, especially children. Poor nutrition can affect oral motor skills, growth, and social development. You can work with your doctor to find the best balance between treatment, nutrition, and quality of life.
A registered dietitian nutritionist, especially one who specializes in food allergies or EoE, may be able to help. They will help you compare the nutrition you or your child needs with foods you or your child can eat. This will help to determine if you need to adjust the diet (if possible) and/or add supplements or medical formula.
You will likely work together to create a meal plan. The dietitian should give you meal ideas, a list of foods to eat, and a list of foods to avoid.
Ask your doctor if they have a recommendation for a dietitian. If not, you can search for one at eatright.org/find-a-nutrition-expert.
How Can I Manage the Impact of EoE?
Managing EoE can mean removing foods from your or your child’s diet, buying specialized formulas, managing medicines and treatments, and adapting social plans. It can have a costly impact on social, emotional, and financial health. This can reduce quality of life. People with EoE may be anxious about issues, such as:
- Physical health
- Financial burden of treatment and hospital visits
- The impact on relationships and social life
- Missing school or work due to frequent medical appointments
Understanding the burden of EoE and getting support can help you manage the impact. With management, treatment, and support, people with EoE can live full lives.
Managing Stress and Anxiety
It’s natural to feel stressed and anxious about managing EoE. Some ways to manage stress include:
- Educating people closest to you so they understand what EoE is, what causes it, and how they can help
- Talking with your health care team about impact and where to find resources
- Talking with a counselor or therapist if you’re having trouble dealing with your feelings or stress
- Consulting a dietitian nutritionist who specializes in food allergies and/or EoE
- Using resources, education, and support from a patient advocacy organization such as the Asthma and Allergy Foundation of America (AAFA) and Kids with Food Allergies (KFA)
Medical and dietary treatment alone may not be enough to help you deal with the stress of managing EoE. It’s important that you find additional support and resources. KFA offers several resources to help you manage your child’s condition:
- Asthma and Allergy Foundation of America community – Join our online support community for support for adults with allergic conditions, including EoE, pollen allergy, asthma, and more.
- Kids with Food Allergies community – Join our online support community to talk with other families managing food allergies in an encouraging environment. When you join our community, you’ll also receive notifications about news, research, food recalls, and educational information to help you manage your child’s food allergies.
- Formula/Medical Foods for Food Allergies – Learn more about different types of formula options available, as well as information on what to do if you can’t afford these expensive medical formula foods.
- KFA School Zone – Find information, resources, downloadable handouts, and forms to help you work with your child’s school to manage their EoE. Our School Zone also includes resources for school staff and teachers.
- Safe Eats® Allergy-Friendly Recipes – Search our collection of more than 1,500 recipes that can be made free of several of the most common allergens. You can search to meet your dietary needs or browse by category.
- Allergy-Friendly Foods – Search our collection of allergy-friendly foods from several different allergy-friendly food companies. You can search for foods free of your allergens or by type of food.
Medical Review: May 2023 by Matthew Greenhawt, MD
References
1. EoE. (n.d.). American Partnership for Eosinophilic Disorders. Retrieved May 8, 2023, from https://apfed.org/about-ead/egids/eoe/
2. Hirano I, Chan ES, Rank MA, Sharaf RN, Stollman NH, Stukus DR, Wang K, Greenhawt M, Falck-Ytter YT; AGA Institute Clinical Guidelines Committee; Joint Task Force on Allergy-Immunology Practice Parameters. AGA institute and the joint task force on allergy-immunology practice parameters clinical guidelines for the management of eosinophilic esophagitis. Ann Allergy Asthma Immunol. 2020 May;124(5):416-423. doi: 10.1016/j.anai.2020.03.020. PMID: 32336462.